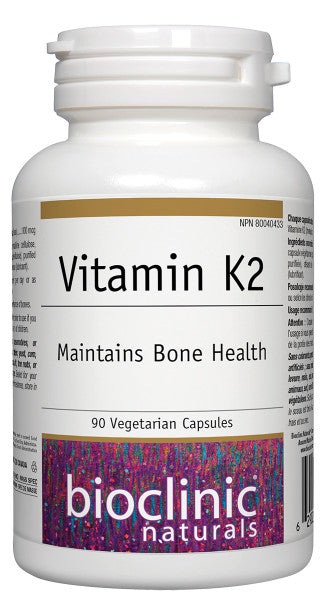
Vitamin K2 · 100 mcg
- 22.99$
0.00$- 22.99$
- Unit price
- per
Description
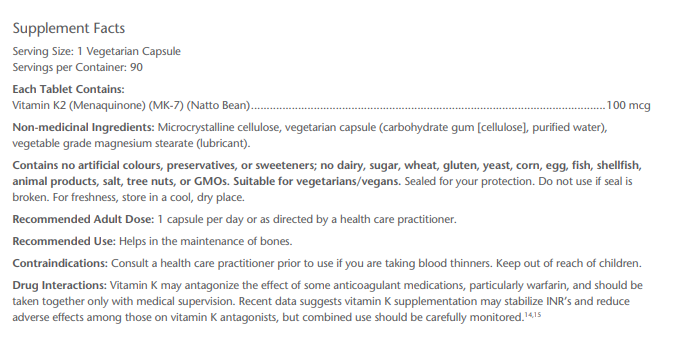
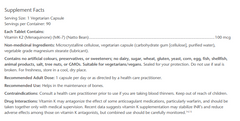
x- Provides 100 mcg per serving of vitamin K2 as menaquinone-7 (MK-7)
- MK-7 has the longest half-life of all forms of vitamin K, as well as the best extrahepatic distribution
- Vitamin K2, particularly MK-7, allows for much lower dosing with significant clinical benefit
- Natto Bean Extract, the richest natural food-based MK-7
- Suitable for vegetarians/vegans
The discovery of vitamin K-dependent (VKD) post-translational modifications of proteins involved not only in coagulation, but also in bone metabolism, vascular calcification, cell growth regulation, and even ATP production has radically changed the physiological and clinical importance of this enzyme cofactor. VKD cofactor proteins are present almost ubiquitously in various cell types, and modification by γ-carboxylation is required for biological activity. Dietary vitamin K intake is often insufficient, and vitamin K is diverted to enzymes essential for short-term survival (e.g., coagulation), leading to suboptimal carboxylation of proteins associated with aging and chronic disease, such as matrix Gla protein, osteocalcin, and gas6.
Clinically, lower vitamin K intake has been linked to a higher risk of myocardial infarction and stroke, plaque instability, and, more recently, diabetes. Higher vitamin K intake, particularly K2, has been associated with lower all-cause mortality, coronary heart disease, aortic calcification, and cancer incidence and mortality. Higher intake of MK-7, which has the longest half-life and the greatest extrahepatic distribution, has been associated with a lower fracture risk and higher BMD.
Produits recommandés
Produits récemment consultés
- Choosing a selection results in a full page refresh.